The things you need to know!
What is a molar pregnancy?
Different types/stages of moles
HYDATIDIFORM MOLE
The commonest kind of trophoblastic disease, where the overgrowth is benign but may spread to other parts of the body if not treated. This is further subdivided into:
PERSISTENT GESTATIONAL TROPHOBLASTIC DISEASE
Where part of the mole remains in any part of the body despite initial treatment by the gynaecologist. Even a tiny amount of mole anywhere in the body can grow quickly and cause problems, so active treatment of this condition is very important.
PARTIAL MOLE
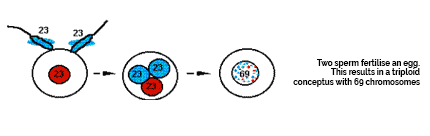
Where part of an apparently normal placenta overgrows (proliferates) and part develops normally. There may be a developing foetus present, but this is genetically abnormal and cannot survive outside the womb. This is where two sperm enter the egg and instead of forming twins forms an abnormal foetus.
CHORIOCARCINOMA
A very rare but curable form of cancer where the placenta becomes malignant. This can arise from a molar pregnancy or an otherwise normal pregnancy or miscarriage. Choriocarcinoma can also spread throughout the body, usually to organs like the lungs, liver and brain.
COMPLETE MOLE
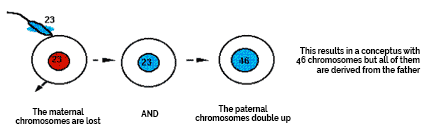
Where the whole placenta is abnormal and usually grows very rapidly. There is no developing foetus in these pregnancies. This is where one sperm enters the egg but only half of one set of chromosomes are present and do not develop into a foetus.
What causes it?
- Age. Risk for complete molar pregnancy steadily increases after the age of 35
- History of molar pregnancy, particularly if you’ve had two or more
- Possible ovulatory disorders
- History of miscarriage
- A diet low in carotene (a form of vitamin A). Women with low carotene or vitamin A intake have a higher rate of complete molar pregnancy
- Living in certain geographic locales (especially Southeast Asia and Mexico)
Prevention
Diagnosis
Complete hydatidiform moles also have a characteristic appearance on an ultrasound scan so this, and the fact that no developing foetus is seen when you have a scan at the ante-natal clinic, can allow the diagnosis to be suspected.
Treatment may be a medical evacuation (tablets are inserted into the vagina and taken orally) or a dilatation and curettage (D & C, or “scrape”) to remove as much of the molar tissue from the womb as possible. This is a minor operation which is carried out after most miscarriages under a general anaesthetic. In most cases, one or two of these minor operations will be enough to remove the mole permanently.
In a normal pregnancy the placenta makes many hormones to support itself, the baby and the mother. One of these hormones is called human chorionic gonadotrophin (hCG), and in a molar pregnancy, where there is overgrowth of the placenta, there is a large amount of this hormone produced.
hCG circulates in the mother’s blood and hCG is excreted in her urine. These can be readily measured in the laboratory from blood or urine samples. This is useful in helping with the diagnosis of the condition, but even more useful in helping decide when a patient is cured. When there is no disease in the body, the level of hCG in the blood and hCG in the urine is low. When there is a lot of disease the level is high. As the disease resolves the levels fall gradually. These tests are important because it is possible to monitor how your disease is progressing.
Please refer to your regional centre for specifics as follow up procedures between centres may differ slightly.
However, as mentioned earlier, even a tiny amount of mole tissue left in the body can grow and spread via your blood stream and this can happen up to many months after apparent cure. Thus your disease will probably be monitored by urine samples for a period of around six months.
However, if the level stays high or starts to rise, this will be detected at the specialist regional centre. The centre will contact you. In some cases drug treatment in the form of chemotherapy is required to eliminate any remaining disease. You are more than welcome to call the centre for your urine results. Up to 10% of women require further treatment in the form of chemotherapy if their hCG hormone levels do not reduce on their own or remain the same.
All this is relatively straightforward. However, because we assess your disease by measuring a hormone normally only seen in pregnancy, if you become pregnant during the course of your follow-up with urine samples, the healthy pregnancy will result in the rapid rise of hCG levels in your urine, which might lead to unnecessary worry and confusion.
Placental site trophoblastic tumour
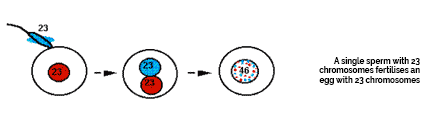
Genetic origin of a Hydatidiform Mole
Monospermic
Involving or resulting from a single sperm cell
Dispermic
The entrance of two spermatozoa into one egg
Normal Conception
Partial Mole
Monospermic Complete Mole
Precautions
Treatment Regimens
Each individual’s case is different but the vast majority of patients begin on Methotrexate. This is also used for arthritis and skin conditions. It is administered by intra-muscular injections (buttock) followed by a Folinic Acid (NOT folic acid) tablet exactly 24 hours later. The usual regimen is to have four injections on alternate days with Folinic Acid in between but regimens differ at different treatment centres. You will stay as an in-patient for the first part of the course of treatment as the chemotherapy could cause heavy bleeding and other side effects. You will then continue as an outpatient either at your treatment centre or it may be possible to arrange it at your local hospital to avoid commuting long distances.
The level of hCG may reach normal (different regions aim for different levels between 2-5) or become undetectable when there is still a residual tumour burden of cells. Therefore with all regimens, treatment is continued for at least six weeks.
Methotrexate Regimen
When returning to your treatment centre on the 1st day of each new course of chemotherapy, you will have several blood tests to measure your blood count, blood platelets, Haemoglobin, liver function and hCG hormones. Depending on your test results and your hormone levels you will be able to continue the Methotrexate programme for another cycle.
This regimen applies only to Sheffield Treatment Centre. For further information on how London Treatment Centre works please contact them directly.
Common known side effects of Methotrexate
It is very important to drink 2 to 3 litres of water every day to flush the toxins from your body from the treatment (this can also come from juice, tea etc).
- Oral mucositis (sore gums and mouth) – Treated with analgesic mouthwash.
- Gritty or runny eyes – Treated with eye drops.
- Pleurisy symptoms – catching sensation on breathing deeply, treated with simple analgesia (on rare occasions this problem can be very severe and may need a change of chemotherapy despite a good fall in hCG levels).
Further treatment
Actinomycin D is given intravenously and repeated every 2 weeks.
Side effects:
Generally it is tolerated well with an increase in tiredness compared to the methotrexate.
- Hair thinning: you do not experience total hair loss and the hair fully recovers after the end of treatment.
- Nausea and vomiting: treated with simple anti sickness drugs
- Constipation: this is usually caused by the side effects from the anti-sickness medication and you will be given stool softeners and laxatives
Duration of follow-up procedures
This regime applies only to Sheffield Treatment Centre. For further information on how London Treatment Centre works please contact them directly.
Cure rate of Molar Pregnancies
If metastatic (disease in other parts of the body) trophoblastic disease is vigorously treated, the cure rate is also 100%.
Widely metastatic disease if recognized promptly and treated aggressively with multi-agent chemotherapy (cocktail) and surgery, the cure rate is about 98%.
Further pregnancies
You may be especially concerned about becoming pregnant again in the future. However, it is highly unlikely that you will suffer another molar pregnancy. In fact, the chance of experiencing a second molar pregnancy is only about 1 in 100. The vast majority of couples go on to have healthy babies.
This is the standard remission time but each individual is different.
Emotions and molar pregnancies
For most women the emotional healing takes much longer than the physical healing from surgery. Even if the pregnancy ended very early, the sense of bonding between a mother and her foetus is often very strong. The feelings of loss can be extremely intense for some couples.
Grief can involve many feelings. One may find oneself looking for reasons why the pregnancy ended. You or your partner may wrongly blame yourselves (or secretly each other). Sickness can manifest itself in the form of headaches, loss of appetite or tiredness. There may be problems with concentrating or sleeping.
Never underestimate unexplained miscarriages, and having to cope with a Molar Pregnancy on top of this is shattering. For those diagnosed with a complete molar they have to come to terms that there was never an embryo or baby. This can be quite destroying especially when the body produces all the normal signs of being pregnant. Although painful, still acknowledge that you conceived and that you and your partner still created something. And if it helps hold a ceremony/memorial for your lost one (no matter how early or late into pregnancy you were) for closure. It will be hard if you are receiving treatment months down the line. Maybe consider it once your treatment has finished then you don’t have that constant reminder of what has happened.
The feelings of grief are usually different between the man and woman; after all, it is the woman that has felt the physical changes of pregnancy.
Talking to each other in a very honest manner is the best way for a man to assist both his partner and himself in the recovery process. Letting her know that she is not alone in her grief can be a true comfort for her. Crying together, explaining yourself and listening to your partner may help on the road to recovery for the both of you.
If either of you are having trouble handling your feelings, try talking to your doctor or close friends or family or even a qualified counsellor. They may not understand your condition but sometimes it helps to talk to someone neutral who can have an objective view on your situation.
Most importantly of all, don’t blame yourselves for the pregnancy loss.
An early pregnancy loss does not mean that you cannot have any more children. The vast majority of women that suffer an early pregnancy loss have a healthy pregnancy later, but do not rush to your decisions too quickly, be sure that both of you are emotionally healed and strong enough to make another attempt.
Adjusting to a loss
What if I require further treatment, will I lose my hair?
Hair loss can be very discouraging and very depressing, especially for a women whose hairstyle is one of her main features. Many support groups offer advice. You will be entitled to a range of NHS wigs with a free prescription for £50-£55 or you can choose to wear a groovy scarf or hat. It is your choice.
Losing you hair may be a small price to pay to be well but do not underestimate the trauma. Try not to be too brave – it is a very real loss; therefore it is natural and understandable for you to take a while to come to terms with losing your hair, if you do come to terms with it. Try not to withdraw from social life and friends, they will want to help and support you.
Contacts
Trophoblastic Screening & Treatment Centres
All three centres offer counselling and support. Contact the centre to ask about this.
